Small service achieves big: Orkney’s journey to GOLD
This case study has been developed by Louise Brewer – Infant Feeding Improvement Specialist Health Visitor, with the support of Janet Dalzell – UNICEF UK Baby Friendly Initiative Professional Lead for Scotland, and the team from NHS Orkney.
About NHS Orkney
An archipelago of over 70 islands, Orkney poses unique geographical barriers for the health professionals tasked with caring for its rural population.
“Most residents live on the mainland, but island communities can range from 70-700 people accessible by a 15-minute flight or two-hour ferry. We face remote challenges being away from mainland services, with our staff taking on extra roles,” shares Louise.
The maternity ward, known as ‘The Maty’, provides prenatal, antenatal, perinatal and postnatal care with two birthing suites, a birthing pool and two rooms for families. Fertility and ultrasound services are supported by three consultant obstetricians.
“There is no neonatal unit, resident paediatrician or neonatologist, so some babies are transferred off-island. In contrast, our health visiting service has three bases to serve all mainland and outer residents.”
The journey to GOLD and key achievements
For NHS Orkney, the journey to GOLD has meant embedding a quality improvement approach to maintaining compassionate mother- and baby-centred care.
“Our goal was to develop robust systems of working to encourage staff to collaborate innovatively across services. The Baby Friendly culture and ethos underpins all our work, and our staff feel proud to provide responsive and compassionate care. Celebrating improvements, big and small, and having the recognition that mothers, babies and their families here in Orkney feel supported, listened to and cared for is hugely satisfying. We’re proud to maintain 100% skin-to-skin rates and have seen breastfeeding rates improve from 61% in 2011 to 73% in 2021.”
A key element of this success has been embedding the four themes of the Achieving Sustainability standards – Leadership, Culture, Monitoring and Progression. Use the drop-down tabs below to learn more.
Implementing new roles
“Progressing Baby Friendly has been difficult at times due to competing clinical priorities, however introducing new roles has been an integral part of achieving GOLD. Having a dedicated Infant Feeding Advisor and Infant Feeding Lead (funded through Scottish Government Programme) helps us understand what we do well, where we can improve, and how to keep up with training and audit.”
“The standards highlight the importance of having board level representation and leadership. Our Baby Friendly Guardian ensures that our Board and Health and Social Care Partnership see Baby Friendly as worth investing in, and our Baby Friendly Lead supports our curriculum of learning. Together, these roles help us to continually innovate and drive improvements within services.”
Maintaining a compassionate and caring culture
“We’re always proud to provide sensitive and bespoke support to our communities. However, this is not without its challenges. At times, lack of dedicated staff time to oversee implementation of the Baby Friendly standards and ongoing clinical commitments have meant that ensuring training and audits are completed, analysed and acted upon has felt burdensome.”
“Notwithstanding, engaging staff and recognising their passion and commitment is important. Our Board Chair and Guardian is a passionate advocate for Baby Friendly and has championed this within our Health and Social Care Partnership. This has been a strength at a time when social care services have undergone improvements. This has meant that even during the pandemic when services were offered in different ways, we could continue to improve and develop.”
Improving culture and overcoming assumptions
“As a small service constantly communicating across teams, it can be easy to simply assume we are progressing with Baby Friendly, without much evidence beyond audits and positive feedback from service users. The following innovations are useful in supporting the culture of our service and helping staff engage with and get a deeper understanding of the Baby Friendly standards:
- Dedicated Baby Friendly meetings to discuss current challenges and new ways to support women to meet their feeding goals
- Improving communication amongst key professionals such as primary care, the dental health team and the third sector to raise awareness about how Baby Friendly positively shapes culture
- Developing an active social media presence to promote Baby Friendly values within our services
- Disseminating a quarterly newsletter to keep staff informed and to highlight great practice
- Promoting staff views and voices at meetings and during training, including encouraging staff to develop their skills and pursue their interests.”
Prioritising regular staff training and education
“We use a range of engaging approaches when it comes to training, such as full-days, short days, hour sessions and bespoke sessions. This helps bring teams together to foster closer relationships, celebrate what we do well, and look at ways to improve.”
“The Baby Friendly framework and tools are helpful for senior staff and managers to see the impact on individual care. We support staff to attend the Baby Friendly Breastfeeding and Relationship Building and Train the Trainer courses to ensure staff education is sustainable over the long term.”
Identifying challenges and shaping support
“Having the support of the Scottish Breastfeeding Leadership Team and using national data collection tools and quality improvement methodology are invaluable in monitoring progress and assessing whether changes to practice make a difference. Because our numbers are small, we are able to follow individual journeys, including those where the outcomes were not as hoped for. From here, we can analyse how we shape support.”
“Ongoing quarterly staff and mother audits mean we can identify challenges and take timely steps to improve the quality of sensitive, individualised care. Auditing our progress going forward will ensure that we continue to deliver the best evidence-based care possible and keep nurturing those relationships.”
Safeguarding against complacency
“Overall, part of Achieving Sustainability has been about improving monitoring and looking for trends and patterns, including assessing how we can shape and improve experiences. Having ongoing, robust monitoring systems in place safeguards against complacency.”
“We use quantitative data from Public Health Scotland and qualitative data from local audits and surveys to inform discussion around priorities for improvement and development. Training for senior staff and regular meetings and reports have meant that Baby Friendly has stayed on the agenda and that senior staff are aware of challenges and steps we are taking to overcome them. Monitoring supplementation rates helps us to look at trends and ensure that training supports all mothers to make an informed choice on how they want to feed their baby.”
Partnering with services and experimenting with new technology
“Continually innovating and progressing allows us to test what works best. During the pandemic, we developed a NHS volunteer peer support service which augments our maternity and community services. This proved useful when faced with staff absence and vacancies, and enabled outreach support to women who went off-island to give birth or access neonatal care. We continue to adapt this service, for example by working with HomeStart who provide peer support with fantastic free resources.”
“We also initially used NHS Near Me technology and video conferencing to provide one-to-one and group support, however we have since developed an in-person weekly walking group that offers support to all parents, regardless of feeding method. This equality of service means that everyone feels valued, and we hope over time this will improve our breastfeeding initiation rates, which are consistently around 80%. In a recent survey of women who received peer support, 100% said they found it helped them to breastfeed. We also reconfigured our antenatal education during the pandemic so we could deliver virtual classes. Parents who attend class are more likely to initiate and continue breastfeeding.”
“Lastly, we have overseen the rollout of the National Breastfeeding Friendly scheme, with many Orkney organisations and businesses joining. We hope this will help drive cultural change over time and increase our initiation rates and reduce attrition.”
Improving standards of care
“Progression is a key part of our journey to GOLD. It’s important for all of us as practitioners to continually improve the quality and standard of our care. We are proud to share that results have been encouraging. Introducing antenatal colostrum expressing to support mothers to feel confident to feed their baby has reduced need for supplementation in some areas, and we take pride in our higher-than-average initiation rates and lower-than-average attrition rates. Looking ahead, having an Infant Feeding Lead in a substantive post would ensure we can continue to shape progression across services.”
We strive for excellence and always aim to improve practice. Baby Friendly gives us the tools and skills to help us on our quality improvement journey, which we embedded into our daily practice from the start. The standards push our team to develop their skills and implement compassionate and baby-centred approaches to infant feeding.
Overcoming challenges
The journey to GOLD has not been without challenges, Louise shares.
“Staffing and recruitment, opportunities for innovation and Covid-19 have disrupted not just innovation and development, but provision of core services, training and audits. Accreditation can feel arduous at times, and opportunities for innovation in infant feeding services can be difficult to find. However, we continue to improve, for example through the use of our NHS volunteer infant feeding peer support service which provides skilled, wrap-around support tailored to the needs of our families.”
Looking ahead
Continuing to strengthen leadership around Baby Friendly and collaborating closely with community organisations are key priorities for the NHS Orkney team.
“Achieving Sustainability has meant focusing on why infant feeding matters and how it improves health and wellbeing. It has provided us with an incredible opportunity to recruit a network of community volunteer peer supporters, truly putting our community at the heart of our Baby Friendly work. Now, I would like to reach even further, developing links with more peer supporters and third sector organisations to build on the hard work and innovation that led to us to GOLD.”
“Developing leadership and ensuring staff and volunteers feel valued, respected and cared for and that families receive high-quality, compassionate, and evidence-based care across services is important to create an Orkney-wide Baby Friendly culture.”
Baby Friendly means my job is about more than meetings, papers, and strategies; it's about women, babies, and families. I've learnt more about the science and evidence base which ensures families have the right support early on to develop happy and healthy relationships, and that they can ask for help from a network of informed, caring practitioners.
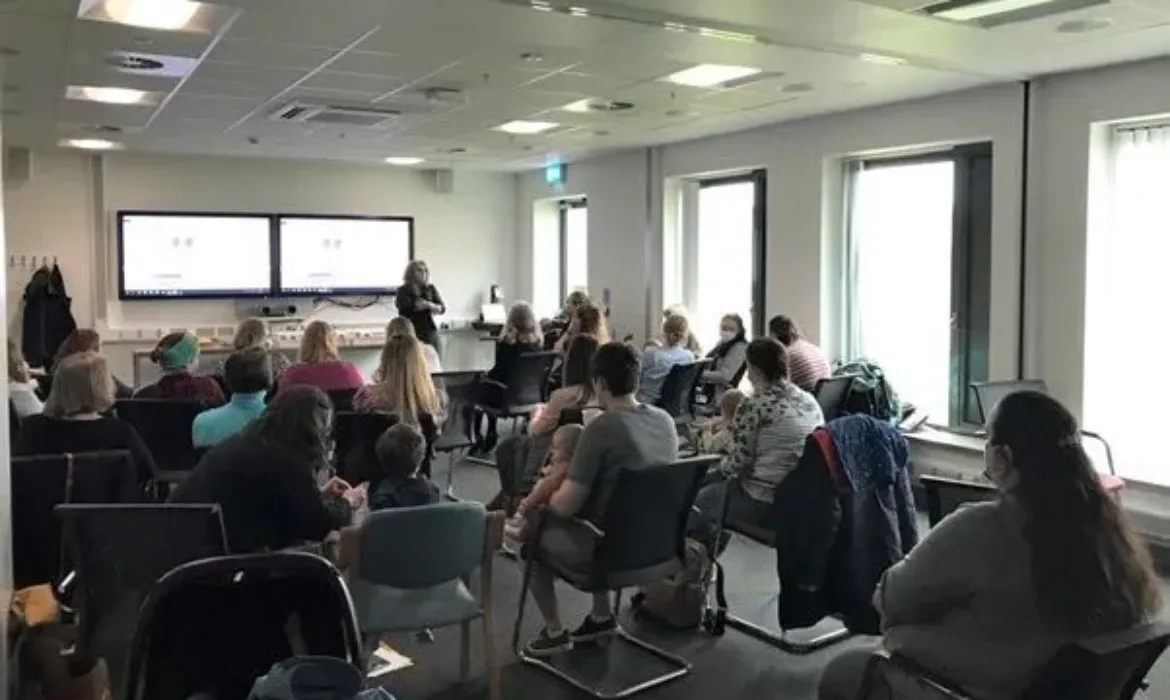
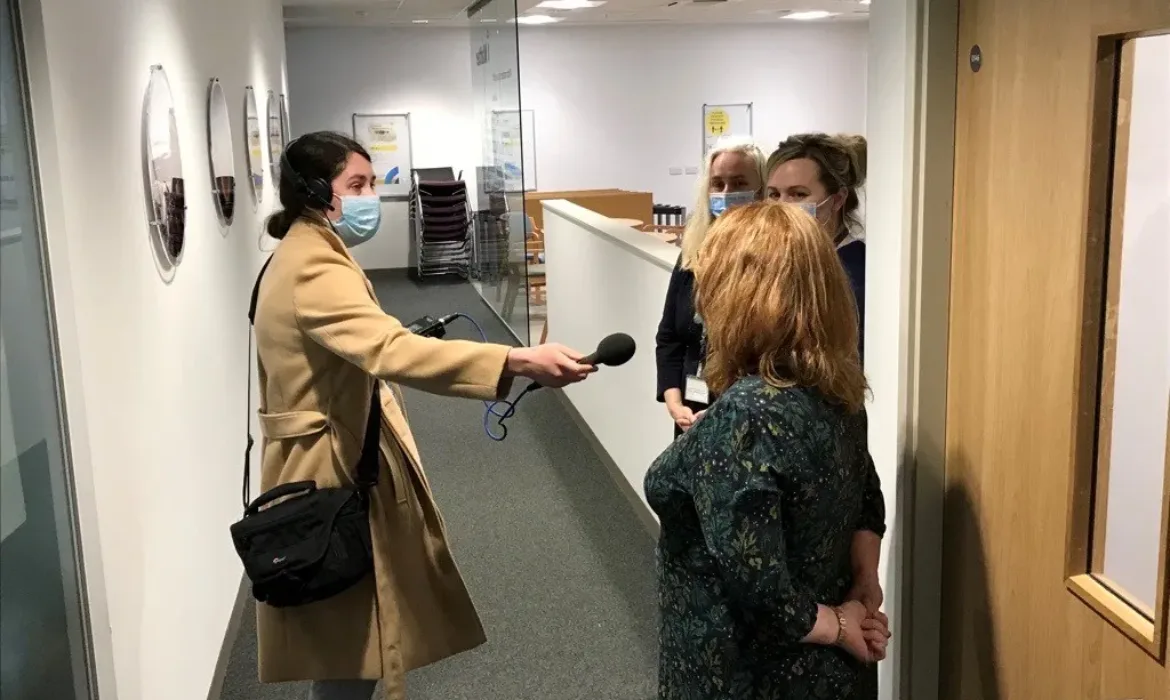
In pictures: GOLD celebration day
Click the arrows to see how NHS Orkney celebrated their award.
Learn about NHS Orkney’s journey to Gold in the module below:
The Baby Friendly ethos extends into all we do to support Orkney families. It's a solid place to begin a journey of improvement, with easy-to-use tools and resources. Our focus continues to be on providing skilled, responsive and nurturing care to babies, their mothers and families. Maintaining GOLD will help us to deliver on this both now and long into the future.
If your service or university is interested in submitting a case study to be featured on our website, please contact the Baby Friendly office at [email protected]