Considering the protection that breastmilk and breastfeeding provide and the minimal role they play in the transmission of respiratory viruses, it is vital that we do all we can to continue to promote, protect and support breastfeeding.
There is a wealth of evidence that breastfeeding reduces the risk of babies developing infectious diseases. Numerous live constituents help to destroy harmful pathogens and boost the baby’s immune system, including immunoglobulins, antiviral factors, cytokines and leucocytes. Breastmilk also protects sick or preterm babies against respiratory infections and necrotising enterocolitis.
Evidence suggests that mothers infected with Covid-19 and those who have received a Covid-19 vaccine pass their antibodies to the virus into their breastmilk, providing protective effects for the baby.
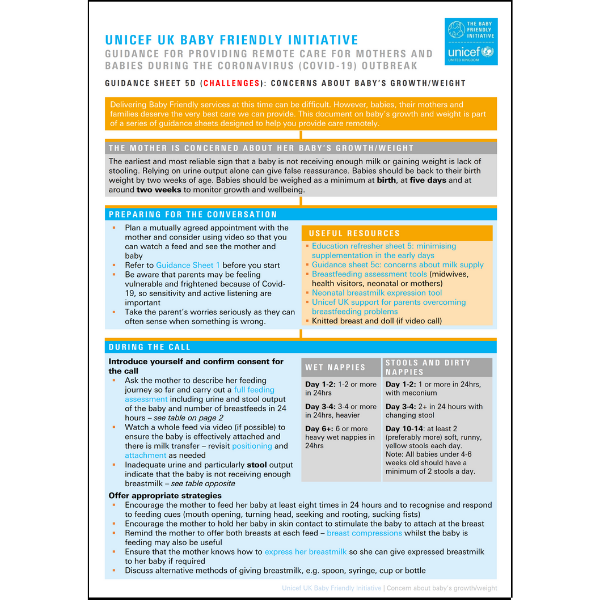
To facilitate expressing and breastfeeding, mothers and babies should be enabled to stay together as much as possible, to have skin-to-skin contact, to feed their baby responsively and to have access to ongoing support and regular skilled assessments. When babies are receiving milk, mothers should be encouraged to maximise the amount of expressed breastmilk they are able to provide. When babies can breastfeed, mothers should be encouraged to give as many feeds as possible. If mothers are considering stopping expressing or breastfeeding, it is worth having a sensitive conversation about the value of continuing during the Covid-19 pandemic.
When mothers are partially breastfeeding, they can be encouraged to maximise the amount of breastmilk they are able to give or, if they choose, to be supported to return to full breastfeeding. If mother’s own milk is not available or needs supplementation, donor human milk is the option of choice, especially for vulnerable infants. Advocating for the use of infant formula to facilitate earlier discharge should be discouraged. Parents who are formula feeding should continue adhering to current guidance on washing and sterilising equipment and should be supported to bottle feed responsively, including pacing feeds and limiting the number of people who feed their baby.
It is recognised that mothers and babies have sometimes been separated in an attempt to curb the spread of Covid-19. However, evidence suggests that this is unnecessary and may be harmful. All pregnant women and new mothers, including breastfeeding mothers, are advised to be vaccinated against Covid-19 as part of the mass vaccination programme.
To help health professionals continue to provide care for babies, their mothers and families, we have produced a series of guidance sheets, education refresher documents and FAQs found below.
Guidance for health professionals
FAQs - updated as new evidence emerges
This can be an anxious time for pregnant mothers who may be worried about the wellbeing of their baby, themselves and their family. Therefore, mothers may appreciate someone to talk to who will listen to their concerns. All mothers should have the opportunity for an antenatal discussion about the value of breastmilk (particularly during the Covid-19 outbreak), getting breastfeeding off to the best start (see meeting baby for the first time) and the importance of skin-to-skin contact. In addition, it is important to discuss with the mother how she can get to know her baby through closeness, comfort and connection and by taking the time to talk, sing and respond to baby’s movements. This can also reduce stress and will be good for the baby’s development.
Yes. There is a wealth of evidence that breastfeeding reduces the risk of babies developing infectious diseases. There are numerous live constituents in human milk, including immunoglobulins, antiviral factors, cytokines and leucocytes that help to destroy harmful pathogens and boost the baby’s immune system. There is currently no evidence that Covid-19 can be passed to the baby through breastfeeding. There is also evidence that mothers with Covid-19 pass their antibodies to their baby through breastmilk, thereby giving protection to their baby. Considering the protection that human milk and breastfeeding offers the baby and the minimal role it plays in the transmission of other respiratory viruses, it is important that we do all we can to continue to promote, protect and support breastfeeding. To facilitate breastfeeding, mothers and babies should be enabled to stay together as much as possible, to have skin-to-skin contact, to feed their baby responsively and to have access to ongoing support when this is needed.
Yes, touch, comfort and communication are vital for the baby’s wellbeing and development (see N. Rollins, 2021). Good hygiene habits are important and will keep the risks to baby as low as possible (see question 4 below). It is also useful to refer to the practical information provided by the UK governments and the World Health Organization (WHO).
This mother should be supported to safely provide her baby with breastmilk in a way that is possible, available and acceptable to her. Consider breastmilk expression by hand/pump and give via a suitable alternative method (see responsive and paced bottle feeding). Maximising breastmilk is important during this time. When the mother is feeling better, encourage skin-to-skin contact and return to full breastfeeding where possible.
Yes. Re-lactation is generally possible and worth trying even if a return to full breastfeeding is not always achievable. Help can be found on the UNICEF UK Baby Friendly guide to maximising breastmilk and supporting re-lactation.
No. There is good evidence that the baby is safer when mothers and babies remain together and practice skin-to-skin contact and rooming in during the day and night, whether or not the mother or her baby has suspected, probable or confirmed Covid-19.
See WHO guidance, New research highlights risks of separating newborns from mothers during Covid-19 pandemic, N. Rollins, 2021)
Yes. Breastmilk is essential for sick and preterm babies as it significantly reduces the risk of serious complications both in the short and long term. Mother’s own milk should always be the first choice as this is responsive to her and her baby’s environment (particularly important during Covid-19). Mother should be supported to express as soon as possible after birth (ideally within 2 hours) and thereafter at least 8-10 times in 24 hours, including at night.
When babies are being cared for on a postnatal ward neonatal unit, parents can be asked to wear a mask when entering and moving around the unit. However, providing that they are asymptomatic, steps should be taken to enable them to interact with their babies without wearing a mask.
Early attachment between the mother (and/or other parent) and baby is critically important for the baby’s wellbeing and development. It is important to support new mothers to keep their babies close to them so that they can respond instinctively through gazing, stroking and talking. Infant cues such as smiling, crying or other facial expressions are powerful motivators of maternal behaviour, helping the mother to communicate and form attachments with her baby. In response, the baby learns to recognise his mother’s face, posture, tone of voice and to form a secure attachment. The baby’s brain grows rapidly from birth and at one year will have developed 70 per cent of its ‘wiring’ for the future and 90 per cent by age three. The development of positive neural pathways is significantly impacted by early parent-infant relationships.
Yes. All pregnant women and new mothers, including breastfeeding mothers, are advised to be vaccinated against Covid-19 as part of the mass vaccination programme.
Useful links and references
A range of Baby Friendly resources on infant feeding and supporting close and loving relationships can be found here. You can also view our dedicated Coronavirus research page.
Telephone support for parents: National Breastfeeding Helpline 0300 100 0212 from 9:30am to 9:30pm, 7 days a week. Live online support via web chat. Information on infant formula can be found at: First Steps Nutrition Trust.
You can also find more information at:
- BAPM Perinatal Covid-19 Resources
- BAPM Human milk and SARS-CoV-2 – A summary of knowledge to date
- BAPM / BLISS Family Integrated Care for Covid-19 – Frequently Asked Questions
- Bliss report: Locked Out: The Impact of COVID-19 on Neonatal Care
- Drug treatments for breastfeeding mothers with Covid 19
- GOV.UK Safer Medicines in Pregnancy and Breastfeeding Consortium
- GOV.UK COVID-19 vaccination: a guide for all women of childbearing age, pregnant or breastfeeding
- GOV.UK – COVID-19 vaccination: women of childbearing age, currently pregnant or breastfeeding
- Hearts Milk Bank
- Journal of Neonatal Nursing: The implications of face masks for babies and families during the Covid-19 pandemic – A discussion paper
- Public Health England – Guidance for households
- NHS: Supporting pregnant women using maternity services during the coronavirus pandemic: Actions for NHS providers
- RCM Advisory Group Optimising mother-baby contact and infant feeding in a pandemic
- Royal College of Obstetricians and Gynaecologists
- Royal College of Paediatric and Child Health
- Start4Life
- UKAMB
- UNICEF Infant & Young Child Feeding in the Context of Covid-19
- WHO FAQs: Breastfeeding and COVID-19 for health care workers
- WHO Infant and young child feeding
- WHO Q&A on Covid-19, pregnancy, childbirth and breastfeeding
- WHO video on Covid-19 and breastfeeding (available in Spanish, Portuguese, Thai, Nepali, Maithili, Bahasa and Japanese)