In this guest blog, Research Associate at DECIPHer, Cardiff University and Senior Researcher for NCT, Heather Trickey, talks us through key lessons from a recent (open access) review of breastfeeding peer support*.
When deciding whether to breastfeed, or considering whether to stop, mothers tend to talk the issues over with close friends and family. Unfortunately, in the UK, many mothers’ social networks have been substantially drained of positive breastfeeding experiences by a history of healthcare practices that have tended to work against decisions to breastfeed and by a wider social context in which breastfeeding is not seen as part of everyday life. Mothers, sisters and friends who want to help can find themselves at a loss.
Breastfeeding peer support aims to fill a gap by linking mothers who want to breastfeed to others who have personal experience and some training. Peer support is recommended by the World Health Organization (pdf) and forms part of UK NICE guidance on maternal and child nutrition and on routine postnatal care. The Unicef UK Baby Friendly Initiative standards require that additional support such as peer support is provided and that services work together to ensure that mothers can get additional help as needed.
Making sense of the evidence
Experiments of breastfeeding peer support have produced mixed results in high income settings. While a Cochrane review (pdf) found that additional lay and professional support improved breastfeeding rates, a systematic review of trials found no examples of effective peer support from the UK.
A difficulty when looking at systematic reviews is that peer support comes in many forms. Peers are recruited and trained to different criteria. They contact mothers at different times. Some interventions are for mothers who are keen to breastfeed, others are for women who are unsure. Intervention settings also vary. Can we really expect peer support to work in the same way in a community where most mothers are still breastfeeding at six weeks, versus one where only one in ten breastfeed for that long? And does it make a difference if the local maternity unit is accredited as Baby Friendly? Or if the local lead volunteer is a human dynamo? What can we learn from such noisy data?
Our realist review sought to improve our understanding by putting 15 one-to-one peer support interventions from the USA, Canada and the UK under the microscope. We learned as much as we possibly could about each intervention case. We studied protocols and process evaluations and talked to the study authors to give ourselves the best chance of understanding why the beliefs and actions of some people in some places changed, while in other places nothing happened. We developed lessons about what works, where, why and for whom; about what needs to happen to give a peer support intervention the best chance of working in any given patch.
A chain of mechanisms
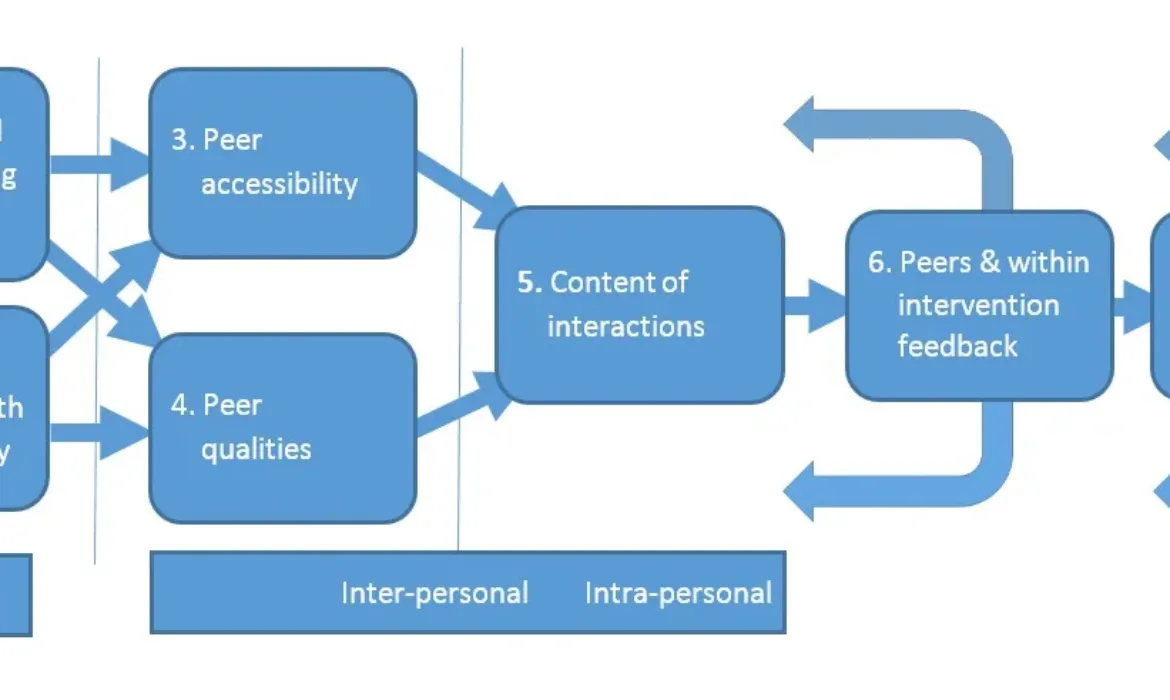
We discovered that breastfeeding peer support relies on a chain of mechanisms firing in sequence (see diagram below). If an intervention design doesn’t address the perceived needs of the target population, if it doesn’t have buy-in from health professionals, if the peer is not accessible or approachable, then it really doesn’t matter how well trained she is, or how good she is at working one-to-one – breastfeeding rates are unlikely to improve.
Fit with local feeding norms
An intervention will not ‘take’ if mothers and key members of her support network don’t think the support is designed for them. Intervention designs may benefit from greater user participation in design and delivery, including a specific stage for community-level participation in agenda setting. Given very low breastfeeding rates in some areas, intervention designs should consider the needs of mothers who anticipate using formula milk, and how these needs can be met within a broader context of breastfeeding promotion and support. Designs could also incorporate intermediate goals, such as changes in social-network-level and community-level knowledge, attitudes and beliefs.
Fit with the healthcare pathway
If health professionals aren’t on board with a goal to improve breastfeeding rates, or are uncomfortable with working alongside peer supporters, mothers will receive mixed messages and the intervention will lose credibility. Ensuring mutual respect and overcoming local barriers to integrated working practices, collaboration and mutual feedback should be a core element of intervention design. Clear role boundaries and referral pathways help. A senior health professional champion can improve the likelihood of successful integration and cross-referral. Identifying and overcoming local barriers should be a specified stage as part of the intervention itself. Baby Friendly accreditation can provide a basis for this kind of effective partnership working.
Accessible help
Support needs to be timely. Peer support around the time of the birth can help mothers who are unsure to firm up decisions to breastfeed. In the UK context, where many mothers stop breastfeeding before breastfeeding is established and where hospital stays are short, peer support needs to be delivered in the first few days. Getting the referral pathways working so that this can happen in practice needs to be a core component for intervention design.
Support also needs to be proactive. Reactive support (as and when requested) tends to be used by mothers who are unusually motivated or unusually confident, and is unlikely to be effective in improving rates overall. This doesn’t mean that support should be untailored; a mother may benefit from adjusting a schedule of contacts to meet her specific needs.
Peer qualities
Mothers value friendly, competent and proactive peers. These qualities seem to outweigh social similarity, although we did find that it helps if peers have personal experience of very specific cultural barriers to feeding. These qualities also seem to outweigh extensive training, though it may be that the impact of training was masked in our findings by upstream factors related to difficulty in accessing support. Peers who feel well integrated and valued by professional healthcare workers are more likely to feel confident in their roles and to exhibit the qualities that mothers value.
The peer-mother contact
Mothers who experience a warm and affirming relationship with their peer supporter often feel helped to overcome challenges and to meet their feeding goals. Relationships that deepen over time are particularly valued, though short term support can also feel enabling. Just knowing that the peer supporter will be in touch can help some mothers overcome challenges.
Antenatal conversations can change specific beliefs about feeding and may help some women who are ambivalent to feel that breastfeeding could be an option for them. Postnatal peer support at just the right time can help a mother to keep going through a difficult patch. However, this timely support may not change her underlying belief about whether she will be able to continue to breastfeed in the longer term.
Peer motivation
Peers are motivated when they feel valued and are demotivated when their offers of help are rejected. As a result, peers tend to focus their energy towards mothers who seek support and who seem to be appreciative. Peers need additional encouragement to persist in contacting and supporting mothers who they perceive to be more ambivalent. We found that peer enjoyment and motivation is improved when peers have opportunities to bond with one another and to learn within their roles.
A lasting impact
Experimental studies tend to focus on individual-level changes; for example, ‘On average, did mothers who received peer support breastfeed for longer?’ Our review suggests there may also be legacy effects from peer support at the level of the healthcare system and the wider community. Legacy effects include changes in the attitudes and beliefs of health professionals, changes in the expectations of local mothers about the care they should receive, and changes in the acceptability and visibility of breastfeeding in the local setting. The potential for peer support to contribute to these wider effects should be considered at intervention design stage and should be integrated into evaluation.
Thinking about future evaluation
The lessons drawn from our review relate to one-to-one breastfeeding support, rather than group-based interventions, and our review does not replace a need for further evaluation. However, the review does raise some issues around how evaluation should be conducted.
Interventions designed for the purpose of experimental study tend to be weakly embedded and prone to implementation failure. As such they are often not a good test of the intervention as it was intended. Given the complex nature of peer support, evaluations should encompass interactions with other aspects of the delivery context and should measure the extent to which peer support is synergistic with existing services, as well as the extent to which it is ameliorating sub-standard care or displacing usual caregivers.
How can peer support contribute to change?
It is important to remember that peer support can only ever be one of a many of influences in any given setting. Ultimately, community-level change in breastfeeding rates will depend on a number of cogs turning together. At present, while researchers and policy makers recognise many influences on infant feeding decisions – at cultural, legislative, organisational, community, social network, family and individual levels – we lack a unifying theory of change to help ensure interventions enable these influences to interact in the most helpful ways. Which cogs should we be turning, in which sequence, to improve breastfeeding rates in the longer term? How can peer support help with that?
These are important questions for researchers to consider. Meantime, we recommend that those commissioning and designing one-to-one peer support interventions draw on the findings of our review to increase the chance of successful delivery.
*The findings presented here are taken from: Trickey, H., Thomson, G., Grant, A., Sanders, J., Mann, M., Murphy, S. and Paranjothy, S., 2017. A realist review of one‐to‐one breastfeeding peer support experiments conducted in developed country settings. Maternal & child nutrition. This research paper is open access.